Tooth pain can be confusing. One day it’s mild sensitivity, and the next it feels swollen, throbbing, or impossible to ignore. Many patients ask the same question: Is this just an infection, or do I need a root canal?
Understanding the difference between an infected tooth, a tooth abscess, and a root canal infection can help you act quickly—and potentially save your tooth.
At Eastern Idaho Endodontics, we see patients every week who waited longer than they should have, simply because they weren’t sure what their symptoms meant. This guide explains what to watch for and when treatment becomes urgent.
What Is a Root Canal Infection?
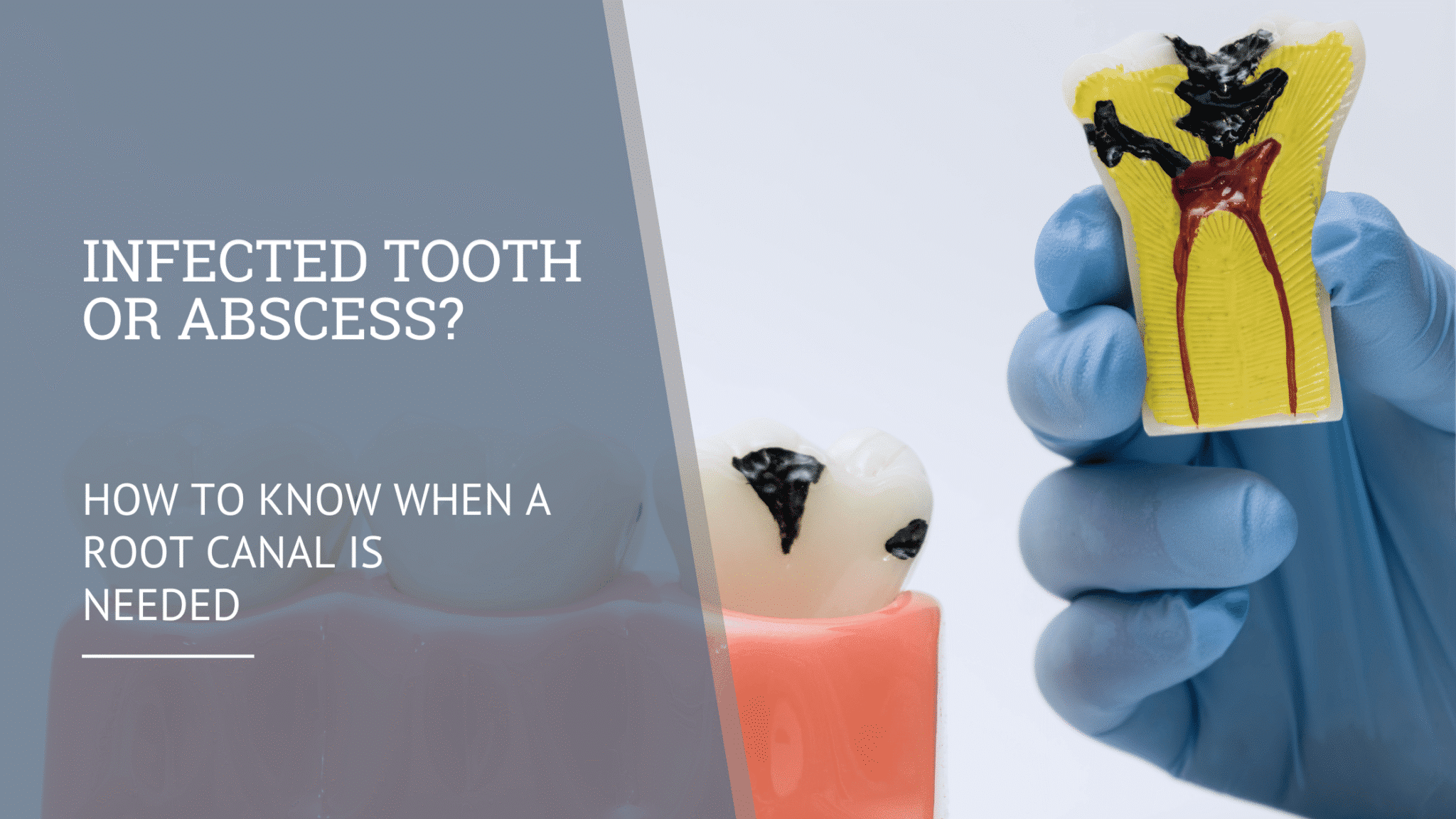
A root canal infection occurs when bacteria reach the soft inner tissue of the tooth, called the pulp. This usually happens when a cavity, crack, or old dental work allows bacteria to travel deep inside the tooth.
Once the pulp becomes infected, the body cannot heal it on its own. Without treatment, the infection can spread beyond the tooth and lead to more serious complications.
Common causes include:
-
Deep tooth decay
-
Cracked or fractured teeth
-
Trauma to a tooth
-
Failed or leaking dental restorations
Infected Tooth vs. Tooth Abscess: What’s the Difference?
Many people use these terms interchangeably, but they are not the same.
Infected Tooth
An infected tooth means bacteria have entered the pulp and begun damaging the nerve tissue. Pain may come and go, and swelling may be mild at first.
Tooth Abscess
A tooth abscess occurs when the infection spreads beyond the tooth root into the surrounding bone or gum tissue. This creates a pocket of pus and often causes more severe symptoms.
In simple terms:
-
An infected tooth can lead to an abscess
-
An abscess is a sign the infection has progressed
Both conditions usually require root canal treatment to stop the infection.
Infected Root Canal Symptoms You Shouldn’t Ignore
Some symptoms are subtle, while others signal an urgent problem. Pay close attention if you experience any of the following infected root canal symptoms:
-
Persistent or throbbing tooth pain
-
Pain that worsens when biting or chewing
-
Sensitivity to hot or cold that lingers
-
Swelling in the gums, face, or jaw
-
A pimple-like bump on the gums
-
Bad taste or drainage in the mouth
-
Tooth discoloration or darkening
If swelling is present, the infection may already be spreading.
Root Canal Swelling: Why It Happens
Root canal swelling occurs when the body responds to infection by sending fluid and immune cells to the area. This pressure builds inside and around the tooth, causing tenderness and visible swelling.
Swelling can:
-
Be localized near the tooth
-
Extend into the cheek or jaw
-
Feel tight, warm, or painful
Facial swelling should always be evaluated promptly, as it may indicate a more advanced infection.
How a Root Canal Treats the Infection
A root canal removes the source of the infection rather than masking symptoms. During treatment, an endodontist:
-
Removes infected pulp tissue
-
Cleans and disinfects the canals
-
Seals the tooth to prevent reinfection
Once the infection is removed, swelling and pain typically improve quickly. In many cases, a root canal saves the natural tooth and prevents the need for extraction.
When Is a Root Canal Urgent?
A root canal becomes urgent if you experience:
-
Swelling in the face or jaw
-
Fever combined with tooth pain
-
Rapidly worsening symptoms
-
Difficulty chewing or opening your mouth
Delaying treatment can allow the infection to spread to surrounding tissues, the jawbone, or even other areas of the body.
Can Antibiotics Fix a Root Canal Infection?
Antibiotics may temporarily reduce symptoms, but they do not eliminate the source of infection inside the tooth. Once bacteria are inside the pulp, only root canal treatment or extraction can fully resolve the problem.
Relying on antibiotics alone often leads to recurring infections.
When to See an Endodontist
If you suspect a tooth abscess or root canal infection, early evaluation matters. Endodontists specialize in diagnosing and treating infections inside the tooth, often saving teeth that would otherwise be lost.
Seeking care early usually means:
-
Less discomfort
-
Faster recovery
-
Better long-term outcomes
Final Thoughts
An infected tooth or abscess is not something to wait out. Root canal infections do not heal on their own, and early treatment can make all the difference.
If you’re experiencing ongoing tooth pain, swelling, or signs of infection, a prompt evaluation can help protect your health—and your smile.
Frequently Asked Questions
Can a tooth abscess heal without a root canal?
No. While symptoms may temporarily improve, the infection remains without proper treatment.
Is swelling always a sign of infection?
Swelling often indicates infection, especially when paired with pain or tenderness.
How quickly should I seek treatment?
If symptoms persist more than a day or worsen, you should be evaluated as soon as possible.
Does a root canal stop the infection completely?
Yes. When performed properly, a root canal removes infected tissue and prevents recurrence.
Is a root canal safer than extracting the tooth?
Saving the natural tooth is usually the healthiest long-term option when possible.